
LEVEL 3 - THE CLINICIAN'S SERIES
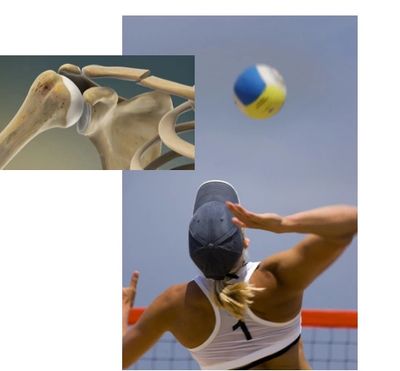
The Athletic Shoulder
Diagnosing and treating athletic complaints can be particularly challenging with 'buried' pathology and treatment resistant outcomes.
We look closely at subacromial, SLAP, ACJ and GHJ disorders affecting adolescent through to senior athletes.
Level 3 - the athletic shoulder
MTS™ Level 3 is a deeper look at difficult athletic injuries, requiring significant analysis, imaging challenges and the need for incorporating multidisciplinary management to offer better solutions and a return to high athletic performance.
Physiotherapy is often critical in helping the patient navigate rehabilitation options, injection management and surgical recommendations for a successful return to sport outcome.
Day 1 will focus on subacromial pathology & SLAP disorders including cuff tendinopathy, acute and chronic bursitis, biceps pathology and atraumatic / traumatic changes when exposed to high athletic use. These disorders are prevalent in all age groups, from late adolescence to senior athletes.
This section will include imaging vs surgical findings, injection strategies and physiotherapy management. What exercises are effective and when to increase or decrease loading for athletic recovery.
We'll look at ACJ pathologies outside of instability (Level II) and how to devise a treatment plan when trying to solve 'impingement' symptoms from several possible components.
Day 2 is dedicated to managing mild - moderate GHJ osteoarthritis and post operative outcomes for shoulder replacements. Athletes that have a dislocation history (dislocation arthropathy) or high load history have much higher risks of developing symptomatic arthritis.
We'll review how it presents and how best to examine and grade OA changes. You'll learn how to guide your patient through decisions from physiotherapy management (including recommended clinical protocols), injection strategies and surgical options.
The afternoon session will cover all shoulder replacements, key pearls and pitfalls for rehabilitation and return to exercise and sport considerations. Total shoulder replacements (TSR) and reverse TSR will be compared with indications, differences in mechanics and what good outcomes look like.
All sessions include lecture, case studies, group discussion and practical components.
Please note: *This course can taken before MTS™ Level II - The Unstable Shoulder*
Created For Physiotherapists
Recommended for :
- All private practice physios
- Senior therapists
- Graduate teaching staff
- Advanced practice physios
- Extended scope physios
- Sports medicine physicians
Pre-requisites
- Level I MTS course only
Course Fee
- Early Bird $1,295 CAD (> 45 days)
- Regular $1,495 CAD (45 - 14 days)
- Final $1,695 CAD (<14-7 days^)
^Please note: Course registration closes @ 5pm PST the Saturday prior to the course date.
Level 3 syllabus - the athletic shoulder

Day 1 - MTS™ Level 3 - the athletic shoulder
TOPIC 8 - SUBACROMIAL & SLAP DISORDERS
- Examination of the Athletic Shoulder
- Bursal, Cuff & Biceps Disorders
- Acute vs Chronic inflammatory patterns
- Acute Inflammatory Bursitis management
- Cuff Tendinopathy - does it produce pain ?
- SLAP lesions of the shoulder
- Managing pain symptoms
- Exercise corrections
- Strength & conditioning recommendations
- Managing effective rehabilitation
Practical Session
TOPIC 9 - IMPINGEMENT OF THE SHOULDER
- Impingement - where are we at ?
- Subacromial, subcoracoid and internal impingement
- ACJ considerations - what to look for
- A deep dive on plain films
- Key findings in US & MRI
- Solving impingement symptoms
- Injection & Surgical options
Case Studies

Day 2 - MTS™ Level 3 - the athletic shoulder
TOPIC 10A - MILD - SEVERE GHJ OSTEOARTHRITIS
- Physiotherapy & Medical Strategies
- Clinical vs radiological findings
- Copycat pain drivers
- Exercise strategies for mild-mod GH OA
- Injection management outcomes
- Resistance training and clinical pearls
Practical Session
TOPIC 10B - END STAGE OSTEOARTHRITIS
- Surgical & Post Op Strategies
- Mod-severe GH OA options
- Hemi arthroplasty & interposition surgeries
- Total Shoulder Arthroplasty (TSA) vs rTSA
- Rehabilitation pearls
- Outcomes and athletic options
- Key rehabilitation technqiues
Case Studies
Learning objectives - the athletic shoulder
Bursal, Cuff & Biceps Tendinopathy
- Understand the identifying features of bursal, cuff and biceps pathology
- Use current and novel special tests to help separate the disorders
- Learn how to treat acute and chronic bursal changes
- Demonstrate exercise strategies for improving cuff and biceps tendinopathy
- Appreciate treatment resistant disorders and injection / surgical options
- Discuss the surgical options and rehab sequencing for better outcomes
Solving Impingement Disorders
- Understand the development and key insights of impingement disorders
- Learn key elements of plain films that may not be reported in radiology
- Recall recommended soft tissue techniques and exercise strategies
- What to look for in US and MRI investigations
- Analyze other options for impingement related symptoms
- Make informed decisions regarding current injection strategies
- Understand the surgical options, errors and pitfalls for impingement disorders
Glenohumeral Osteoarthritis - Non-surgical Rehabilitation
- Recall the common symptoms for GHJ OA
- Appreciate radiological and clinical signs of OA and functional grading
- Learn special tests to identify symptomatic OA
- Understand the rationale for mild-moderate OA physio treatment
- Make correct choices in exercise progressions for OA
- Be able to advise on injection choices for joint preservation and pain relief
Glenohumeral Osteoarthritis - Post Surgical Management
- Be able to explain the choices and reasoning for various surgical options
- Describe the differences in mechanics and movement for TSR & rTSR
- Advise on the exercise limits and precautions for TSR & rTSR
- Understand the early and late complications of TSR & rTSR
- Be able to describe critical milestones of rehabilitation
- Appreciate the ongoing improvements in TSR and rTSR based on the history of design
2026 REGISTRATION OPEN
LEVEL 3 Q&A
Bursal, Cuff & Biceps Tendinopathy

- How does acute vs chronic bursitis management differ ?
- How is cuff tendinopathy measured ?
- When is cuff tendinopathy symptomatic ?
- Can you clinically test for cuff tears ?
- What are the normal cuff changes related to age ?
- What is swimmer's shoulder ?
- What is the ideal progression for cuff tendinopathy ?
- Can you solve chronic bursitis with exercise methods ?
- How do you keep the shoulder pain free ?
Solving Impingement Disorders

- Where is the research at ? How successful is physiotherapy ?
- What problems are we looking for ?
- Are there particular x-rays that are important ? Will it be reported ?
- What should you look for on US and MRI/A reports ?
- Are there clinical tests that are helpful to use ?
- What are the sports medicine options ? Surgical options ?
- How, where and how often should injections be applied ?
- Is there a role for dry / wet needling ?
- What should a patient ask a surgeon and how do you avoid poor outcomes ?
Glenohumeral Osteoarthritis
Glenohumeral Osteoarthritis
Glenohumeral Osteoarthritis

- What are the differentials for GHJ osteoarthritis ?
- Is it important to see the films directly ?
- What are the key measures for grading GHJ OA ?
- Are there exercise choices to avoid in mid stage OA ?
- What are the recommended movements for reducing OA pain ?
- How should exercise be progressed ?
- What is the role of injection work ? How often and what injectables are best for the shoulder ?
- Are manual therapy techniques useful for pain relief ?
- Are EPAs effective for pain relief ?
- How do you maximize function of the GHJ OA shoulder ?
Total Shoulder Arthroplasty
Glenohumeral Osteoarthritis
Glenohumeral Osteoarthritis

- What determines the choice of shoulder replacement ?
- How good are the outcomes for hemi, interposition and total joint surgeries ?
- Explain the key rehabilitation issues for reverse TSR (rTSR) ?
- What type of movement is normally seen in reverse prostheses ?
- What are the early and late complications of replacements ?
- What do you need to know from the surgeon ?
- How do you avoid joint stiffness for TSR and rTSR ?
- What are the ideal range of motion goals ?
- Are there particular precautions for both surgeries ?
- What are the limitations for sport and exercise ?
LEVEL 3 CASE EXAMPLE
39 y/o female competitive athlete with restricted shoulder rotation and pain
A competitive volleyball player has noticed increasing shoulder pain on serving, blocking and spiking for the past 4 months. The symptoms have been ongoing for the past 3 years, and a full season of rest, two weeks of anti-inflammatories and regular icing has not improved the concern. She regularly strength trains and has seen several therapists without improvement. She is considering a PRP injection with her sports medicine doctor.
Examination reveals a mixture of positive subacromial, bicep and ACJ tests. Rotational movements in flexion create high sensitivity. X-rays are reported as normal, a recent US demonstrates some bursal thickening and no cuff tears visible. Posterior joint and suprascapular notch are clear. MRI shows some distal clavicle edema, no cuff tear, type II acromion and no obvious labral pathology.
- Cuff and overhead exercises make the shoulder sore - how would you proceed ?
- What parts of the current investigations would you need to confirm ? What could you be looking for ?
- Are there manual therapy and exercise choices that are likely to help ?
- What clinical tests would be helpful in determining injection choices ?
- What advice would you give for return to training, play and competition ?
- What might the surgical remedies look like and how should they be approached for best outcomes ?
- What are the likely points to consider between management and curative solutions ?
Keep me updated
Copyright © 2014-2026 ShoulderPT - All Rights Reserved.
